2016 Personal Breast Cancer Surgical Activity Analysis
Choosing your breast cancer surgeon is a very important decision, as not only may it influence the range of surgical options you are offered, but your breast surgeon acts as the “gatekeeper” to your entire specialist multidisciplinary breast cancer treatment team. (1)

It is useful and informative for breast surgeons to regularly undertake a formal assessment and analysis of their surgical activity for breast cancer, and in my opinion, this information should ideally be available to existing and potential patients.
An audit of the twelve month period Jan- Dec 2016 revealed the mastectomy rate (40%) to be similar to recent previous years and the immediate reconstruction rate continues to increase (84%).
For patients undergoing surgery for breast cancer (including both invasive and preinvasive malignancy) in 2016, 60% successfully underwent breast conserving surgery (wide local excision/WLE) and 40% underwent mastectomy.
Breast Conserving Surgery
- 70% patients overall underwent intial breast conserving surgery.
- 14% of these women ended up having mastectomy, 55% of whom elected to proceed with mastectomy by choice ie satisfactory pathological margins. Of the remaining 45%, 75% of these women underwent eventual mastectomy after margin reexcision failed to achieve satisfactory pathological margins and 25% proceeded directly to mastectomy after initial wide local excision margins were involved.
- Only 6% patients undergoing initial wide local excision, ended up having a mastectomy because of unsatisfactory margins either at initial lumpectomy or following margin reexcision.
- Of the 60% patients who successfully underwent breast conserving surgery, in 22% of these, it was in conjunction with some form of oncoplastic procedure.

Neoadjuvant (preoperative) Chemotherapy
- 11% patients underwent preoperative chemotherapy (neoadjuvant chemotherapy-NAC) prior to surgery.
- In 40% of these women, the indication for neoadjuvant chemotherapy was LABC (locally advanced breast cancer) with either an inflammatory breast cancer or generalised skin oedema).
All women with LABC proceeded following completion of chemotherapy with preplanned mastectomy without reconstruction.
In the remaining 60%, all of whom had “operable” breast cancer at diagnosis, neoadjuvant chemotherapy was undertaken in the context of a potentially “chemosensitive” subtype ie triple negative breast (TNBC) or HER2+ve.
In 60% of these operable cases, successful downstaging occurred, allowing successful breast conserving surgery.
- 1 patient (TNBC) progressed on NAC, which was discontinued, and mastectomy with recon performed
- 1 patient underwent bilat mastectomy (patient choice)
- 84% of patients undergoing mastectomy for malignancy underwent immediate reconstruction.
- 32% patients undergoing mastectomy for malignancy underwent bilateral mastectomy.

For patients undergoing surgery for breast cancer
- 63% Melbourne metropolitan area
- 34% regional Victoria
- 2% interstate
Risk-Reduction Mastectomy
- All patients (100%) undergoing risk-reduction mastectomy underwent immediate reconstruction.
- 100% implant based reconstruction.
- 100% One stage- direct-to-implant ( DTI) reconstruction
Patient undergoing bilateral risk reduction mastectomy were aged 22-57 years (median age 30 years)
All but one patient was a proven BRCA mutation carrier.
For patients undergoing risk-reduction surgery
- 50% from interstate
- 33% from regional Victoria
SUMMARY:
Patients undergoing surgery for breast cancer (including both invasive and preinvasive malignancy)
Breast Conserving surgery -60%
- 22% in conjunction with oncoplastic procedure
Mastectomy -40%
- 84% in conjunction with immediate reconstruction.
- 32% of all patients undergoing mastectomy for malignancy underwent bilateral mastectomy
- 48% of Mx with immed recon were nipple sparing procedures, 53% of which were bilateral. Of the remaining 52% (skin sparing procedures) only 25% were bilateral.
Bilateral Mastectomy
- 13% of all breast cancer patients
- 32% of patients undergoing mastectomy
Immediate Reconstruction (rate 84%)
- 74% -Implant Based Recon
- 26% – Autologous Tissue Reconstruction
Implant Based Recon
- 83% – Single Stage -Direct-to- Implant (DTI) usually in association with acellular dermal matrix (ADM)
- 17% – Two Stage – Tissue Expander/Implant
Autologous Tissue Reconstruction
- All DIEP flaps

| BREAST CANCER OPERATIONS | 2015 | 2016 |
| Mastectomy Rate (% ) |
36 | 40 |
| Breast Conservation -Wide Local Excision (WLE) % |
64 | 60 |
| Oncoplastic procedure in association with WLE (% of WLE) | 28 | 22 |
| Bilat Mastectomy (% of overall mastectomies) |
28 | 32 |
| Immediate recon (% of Mx) |
78 | 84 |
| Nipple-Sparing Mastectomy (% of mastectomy with immediate recon) |
54 | 48 |
| Autologous Recon (% of overall immediate recon) |
21 | 26 |
| Implant Based Recon (% of overall immediate recon) |
79 | 74 |
| Two Stage Implant Recon (tissue expander/implant) (% of implant recons) |
73 | 17 |
| One Stage Implant Recon Direct to implant (DTI) +/- Dermal Matrix (% of implant recons) |
27 | 83 |

Patients undergoing bilateral risk-reduction surgery
Bilateral Risk-Reduction Mastectomy
- All patients (100%) underwent immediate reconstruction.
- 100% implant based reconstruction.
- 100% Nipple-sparing mastectomy
- 100% one stage- direct-to-implant (DTI) reconstruction
| BILATERAL RISK-REDUCTION MASTECTOMY | 2016 |
| Immediate recon (% ) |
100 |
| Nipple-Sparing Mastectomy | 100 |
| Implant Based Recon | 100 |
| One Stage Implant Recon Direct to implant (DTI) +/- Dermal Matrix (% of implant recons) |
100 |
DISCUSSION:
Jane O’Brien’s mastectomy rate (40%) has remained fairly constant over recent years (2013 35%, 2015 36%, 2016 40%) and the immediate reconstruction rate has continued to rise, 2010-2012-65%, 2014 -73%, 2015-78%, 2016-84%. The exceptionally high immediate reconstruction rate of 84%, against a national average of 9-12% is explained by a number of physician, patient and practice related factors which were explored in some detail in the discussion section of the 2015 activity analysis- http://bit.ly/2mDxvwm
Direct-to-Implant (DTI) (One Stage) Reconstruction with Acellular Dermal Matrix (ADM)
The most striking finding in the current practice activity analysis is the increase in one stage, direct-to-implant (DTI) reconstruction, both in the therapeutic and risk reduction setting. In 2016, 83% of all implant based reconstructions in breast cancer patients were one stage- direct-to-implant (DTI), up from 27% the previous year (2015) and 100% of the risk reduction patients underwent bilateral nipple-sparing mastectomies with immediate one stage, direct-to-implant (DTI) reconstruction.
Direct-to-implant (DTI) reconstruction is a newer technique that is not yet widely available in Australia. It is an alternative approach to the traditional expander-implant breast reconstruction, allowing the placement of a breast implant right after a mastectomy is completed, in one operation.

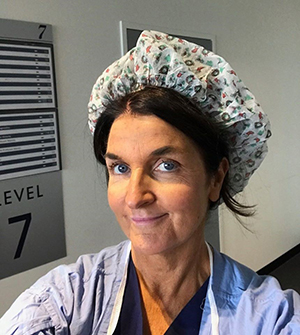
A significant contributing factor to the increase use of this technique is the relatively recent availability of Acellular Dermal Matrix (ADM) and mesh products in Australia, many of which are now funded. DTI reconstruction aims to provide one-step surgery through the use of a specialised surgical mesh (biological Acellular Dermal Matrix (ADM) or prosthetic mesh eg Titanium-coated polypropylene mesh- TiLoop®) to create a sling within the chest that cradles the permanent implant, which is inserted at the same time.
As the surgeon can manipulate the implant position within the sling, the result is a more natural looking breast. The ADM provides a ‘hammock’ that cradles the breast implant, helping to create a natural droop, shape and contour.
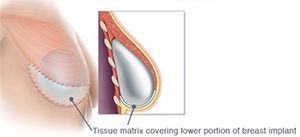
The procedure is suitable for selected women who are having nipple-sparing (or skin-sparing) mastectomies and are seekingimmediate reconstruction. The option of nipple-sparing mastectomy with DTI reconstruction is particularly attractive to younger women with a genetic disposition to breast cancer, undergoing bilateral risk reduction mastectomy.
A DTI procedure has obvious appeal to patient and surgeon alike, but not everyone is a candidate for single-stage reconstruction. The key to success is in patient selection, technique, and intraoperative decision-making.
Patient selection begins at the initial consultation. The history assesses the overall health of the patient and treatment plan, previous surgeries and co-morbidities, current medications, and smoking status. The ideal candidate for DTI reconstruction is an otherwise healthy non-smoker with a small to moderate sized breast, and who desires to be a similar breast size. (2,3)
If a patient wishes to be signicantly larger in size, this is typically more safely done in two stages with tissue expander-implant reconstruction. Patients who have multiple medical co-morbidities that increase the complication risk may be better served with delayed reconstruction.
Active smoking and pre-existing scars on the breast adversely affect skin perfusion and thus DTI may not be possible. The skin of the large breast may also pose challenges as it tends to become more ischemic than the skin of smaller breasts with mastectomy. Therefore, even though there is often an excess amount of skin available to use, reconstruction may need to be done in two stages or it may even need to be delayed.
Even if the patient meets the criteria, and is a candidate for DTI reconstruction, the final decision on DTI is made in the operating room based on the health and perfusion of the mastectomy skin envelope, and the surgeon should be prepared to do a tissue expander reconstruction if required. By limiting the volume of the tissue expander at the initial operation such that the skin envelope is expanded but not under tension, the risk of mastectomy skin flap and nipple-areolar ischaemia is reduced.

The decision to proceed with immediate one-stage or two-stage breast reconstruction depends on multiple factors related to the patient, disease, and treatment. Perfusion to the skin and nipple comes primarily from the breast that must be removed. Thin mastectomy flaps are desirable from an oncological standpoint because leaving fibroglandular tissue behind poses an oncological risk, but the risk of damage to the subdermal vascular plexus, the only remaining source of skin perfusion after mastectomy, is increased, and damage can result in the remaining skin becoming ischaemic and can hinder healing after mastectomy.

Those commonly believed to be the best candidates for one-stage implant reconstruction: young, thin women, with no pre-existing medical comorbidities or history of smoking, who desire reconstructions similar to or smaller than their original breast size.
Although the concept of having everything taken care of in one operation sounds great, and the DTI procedure can be a great option for some women, calling it “one and done” as it is commonly referred to in the USA, can be misleading, as over 30% of women will need further revisional surgery. The main advantage of direct-to-implant breast reconstruction is the elimination of the lengthy, inconvenient and occasionally poorly tolerated tissue expansion process, which can be uncomfortable and requires multiple office visits.

The technique of one-stage direct-to-implant reconstruction with acellular dermal matrix has certainly expanded the surgeon’s repertoire and given carefully selected patients an opportunity to have a one-stage option, especially in conjunction with nipple-sparing mastectomy (NSM). If you are interested in exploring whether the option of a reconstruction incorporating the use of a mesh or ADM is something that may be considered in your case, you should check as to whether your particular treatment team has experience in its use.
For more information on DTI reconstruction see: http://bit.ly/2n6yaTe
- Six Questions for Patients to Ask their Breast Surgeon Before they Undergo their Breast Cancer Surgery
- Rodriguez-Feliz et al. Embrace the Change: Incorporating Single-Stage Implant Breast Reconstruction into Your Practice. Plastic and Reconstructive Surgery, 2015
- Colwell AS. Current strategies with 1-stage prosthetic breast reconstruction. Gland Surg 2015
 Six Questions for Patients to ask their Breast Surgeon
Six Questions for Patients to ask their Breast Surgeon
 Embrace the Change: Incorporating Single-Stage Implant Breast Reconstruction into Your Practice
Embrace the Change: Incorporating Single-Stage Implant Breast Reconstruction into Your Practice
 Current strategies with 1-stage prosthetic breast reconstruction
Current strategies with 1-stage prosthetic breast reconstruction