Audit 2018/ Unilateral/ Bilateral Mastectomy Rates/ Neoadjuvant Chemotherapy

Each year, I perform a detailed audit of my surgical activity for the previous year, which I publish on this webpage and also post on Facebook – www.facebook.com/DrJaneOBrien . I believe that it is useful and
informative for breast surgeons to regularly undertake a formal assessment and analysis of their surgical activity for breast cancer and risk-reduction surgery, and in my opinion, this information should ideally be made available to existing and potential patients. This audit is of the 12 month period Jan-Dec 2018.
For patients undergoing surgery in 2018 for breast cancer (including both invasive and preinvasive malignancy), 52% conserved their breast (wide local excision/WLE/breast conserving ) and 48% underwent mastectomy.
- Breast Conserving Surgery (BCS) /wide local excision(WLE) /lumpectomy- 52%
- Mastectomy (Mx)- 48% (55% Mx unilateral, 45% bilateral)
- Unilat Mx –26% of all cancers
- Bilat Mx- 22% of all cancers
Breast Conserving Surgery (BCS)
- 55% patients overall underwent initial breast conserving surgery.
- 5% of these women ended up having a mastectomy, all of which were bilateral mastectomies with immediate reconstruction.
- All of the patients who elected after initial wide local excision to proceed with bilateral mastectomy had clear pathological margins after the initial wide local excision.
- There were a variety of reasons these women chose to undergo mastectomy, despite clear lumpectomy margins. In several, the malignancy had been either occult (not seen) on initial breast imaging or significantly underestimated on conventional breast imaging.
- No patient undergoing breast conserving surgery had involved margins.
- In 41% patients who underwent breast conserving surgery, it was performed in conjunction with some form of oncoplastic procedure.

Mastectomy
- 48% patients underwent eventual mastectomy.
- 45% of mastectomies overall were bilateral. (55% unilateral)
- 80% patients undergoing mastectomy underwent immediate reconstruction.
Only one woman undergoing mastectomy was not offered immediate reconstruction. This patient was advised to undergo delayed reconstruction following radiotherapy for tumour related reasons (inflammatory breast cancer) - 49% women undergoing mastectomy with immediate reconstruction underwent bilateral mastectomy.
- 30% women undergoing mastectomy without immediate reconstruction underwent bilateral mastectomy.
- 53% of Mx with immed recon were nipple-sparing procedures.
- 90% patients undergoing nipple-sparing mastectomy for malignancy underwent prior nipple-delay
Nipple Delay
Surgical complications related to nipple-sparing mastectomy (NSM) are not unusual. The ability to oxygenate the breast skin is related to the blood supply, and the blood supply to the nipple and areola particularly may be in jeopardy following NSM. Necrosis (tissue death), with either partial or total loss of the nipple +/-areola complex, has been noted in virtually all reported series of nipple-sparing mastectomy. It appears to vary from a high at around 20% to a low of 2-3%, with most series reporting an incidence of around 10%. Many factors account for the differences, including choice of incision, breast size (increased risk in larger breasts) and on how radically the breast tissue from behind the nipple and areola is removed.
To reduce the chance of nipple necrosis, consideration is given to performing a surgical “nipple delay” procedure. “Nipple delay” is intended to create new circulatory connections from the breast skin to the nipple/areolar complex, and involves dividing the blood vessels and other breast tissue beneath the nipple, so that the nipple is no longer dependent on the underlying breast tissue for it’s blood supply. Over the next 1-2 weeks, the remaining blood supply becomes more robust, and the blood flow to the nipple-areola from the surrounding skin increases. The nipple becomes accustomed to receiving it’s blood supply from the skin around it, instead of via the breast tissue underneath, which can potentially help it survive the subsequent nipple-sparing mastectomy procedure. At the time of nipple delay, tissue samples are taken from directly behind the nipple for pathology, to ascertain the oncological appropriateness of retaining the nipple. “Nipple Delay” procedures are performed a week or two prior to nipple-sparing mastectomy.
Bilateral Mastectomy
- 22% of all breast cancer patients underwent bilateral mastectomy
- 45% of patients undergoing mastectomy, underwent bilateral mastectomy
- 49% women undergoing mastectomy with immed recon, underwent bilat mastecomy
- 86% women undergoing bilateral mastectomy, underwent immediate reconstruction
- 58% women undergoing bilateral mastectomy underwent autologous flap reconstruction
| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
| % of overall Mx which were bilateral | 45 | 28 | 28 | 32 | 30 | 45 |
| % Mx/Recon which were bilateral | 54 | 39 | 32 | 36 | 36 | 49 |

Immediate Breast Reconstruction (IBR)
- 80% immediate reconstruction rate
- 82% – Autologous (tissue flap) reconstruction
- 18% -Implant-Based Recon
Implant-Based Reconstruction
- 88% Single Stage -Direct-to- Implant (DTI) in association with acellular dermal matrix (ADM)
- 38% implant based recon–prepectoral placement of prosthesis with ADM
Autologous Tissue Flap Reconstruction
- All DIEP flaps, with the exception of x1 TUG flap (bilateral)
- One pt undergoing quadrantectomy, underwent LICAP flap reconstruction (not included in mastectomy/recon data)
| Breast Cancer Surgery | 2015 | 2016 | 2018 |
| Mastectomy Rate (%) | 36 | 40 | 48 |
| Breast Conservation -Wide Local Excision (%) | 64 | 60 | 52 |
| Bilat Mastectomy (% of overall mastectomies) | 28 | 32 | 45 |
| Immediate recon (% of Mx) | 78 | 84 | 80 |
| Nipple-Sparing Mastectomy (% of mastectomy with immediate recon) | 54 | 48 | 53 |
In 2018, 82 % of all immediate reconstructions were autologous, compared to 57% in 2017, 26% in 2016 and 21% in 2015.

| Immediate Reconstruction for breast cancer (risk-reduction surgery excluded) | 2015 | 2016 | 2017 | 2018 |
| Autologous Recon (% of overall immediate recon) | 21 | 26 | 57 | 82 |
| Implant Based Recon (% of overall immediate recon) | 79 | 74 | 43 | 18 |
| One Stage Implant Recon Direct to implant (DTI) +/- Dermal Matrix (% of implant recons) | 27 | 83 | 83 | 88 |
| Prepectoral (cf subpectoral) implant based recon (% of implant recons) | – | – | – | 38 |
Risk-Reduction Mastectomy
- All patients (100%) undergoing risk-reduction mastectomy underwent immediate reconstruction.
- 67% implant based reconstruction – all nipple-sparing procedures, all single stage-direct-to-implant (DTI) reconstruction.
- 100% patients undergoing bilateral nipple-sparing risk-reduction mastectomies underwent prior nipple-delays.
- 50% of patients undergoing implant based recon (DTI) underwent prepectoral DTI reconstruction with ADM. The remaining 50% underwent subpectoral/dual-plane DTI reconstruction with ADM.
- 33% autologous recon (DIEP flaps). These women, having more generously sized breasts, underwent skin-sparing mastectomies, with reduction of the skin envelope and sacrifice of the nipples.
Patients undergoing bilateral risk reduction mastectomy were aged 28-54 years and 2/3 were confirmed mutation carriers.
Non-Surgical Therapies
It should be noted that the proportion of pts with invasive breast cancer undergoing non-surgical therapies, ie neoadjuvant chemotherapy, adjuvant chemotherapy/radiotherapy are slightly higher than the figures below reflect, as all of these figures include both invasive and preinvasive malignancies.
Chemotherapy
- 45% pts overall underwent chemotherapy.
- 70% of these in the adjuvant (post-operative) setting
- 30% preoperative/neoadjuvant (NAC) chemotherapy
Neoadjuvant (preoperative) Chemotherapy
- 14% breast cancer patients overall underwent preoperative chemotherapy (neoadjuvant chemotherapy-NAC) prior to surgery.
- 30% patients undergoing chemotherapy, received it in the neoadjuvant setting
Year % of all breast cancer pts undergoing NAC 2013 4 2014 5 2015 4 2016 10 2017 9 2018 14 - In 10% of the women undergoing NAC, the indication was LABC (locally advanced breast cancer) with either an inflammatory breast cancer or skin involvement.
- The remaining 90% women had “operable” breast cancer at diagnosis, and neoadjuvant chemotherapy was undertaken in the context of a potentially “chemo-sensitive” subtype ie triple negative breast (TNBC) or HER2+ve.
- 86% of these women subsequently underwent successful breast conserving surgery.
Discussion:
Neoadjuvant treatment offers a number of benefits for patients with early breast cancer, and is an important option for consideration by multidisciplinary teams. Despite literature showing its efficacy, the use of neoadjuvant therapy varies widely. NAC is used in only 3.8% of cases in the United States and in 2.75% of operable breast cancer cases in Australia and New Zealand according to BreastSurgANZ Quality Audit data (5), compared with 14% in Jane O’Brien’s practice in 2018.
In the treatment of women with operable breast cancer, NAC provides a number of potential advantages including: improving the chance of achieving breast-conserving surgery, improving cosmesis after breast-conserving surgery, downstaging the breast and axilla, allowing time to fully consider surgical options, time for genetic testing and facilitating breast reconstruction.
The neoadjuvant chemotherapy (NAC) rate in Jane O’Brien’s practice continues to increase over time. Overall, 30% of the women in 2018 undergoing chemotherapy for early breast cancer received it in the neoadjuvant (preoperative) setting.
Evaluation of the American National Cancer Database from 2010–2015, demonstrated that approximately 20% of patients who received chemotherapy, received it upfront in the neoadjuvant setting, (cf Jane O’Brien -30% in 2018) with the proportion significantly increasing in the USA from 15.7 to 26.0% between 2010-2015. (6)
Adjuvant (post-operative) Therapies
Adjuvant Chemotherapy
- 45% pts overall underwent chemotherapy.
- 70% of these in thee adjuvant setting
- 30% neoadjuvant
In women undergoing mastectomy -52% underwent chemo
- Mx with recon- 55% chemo- 20% of whom NAC
- Mx/no recon- 40% chemo, 50% of whom were NAC
Adjuvant Radiation
Radiation following Breast Conserving Surgery (BCS)
- Post Wide Local Excision (BCS) 83% women underwent radiation
- 17% BCS no XRT- majority were older pts (aged 77-95)
- 2 pts with non-high risk DCIS decided against XRT after meeting with a radiation oncologist and discussing radiation.
- 2 pts with ERPR-ve/HER2+ve disease declined post BCS XRT following NAC. Both pts had achieved PCRs.
Post Mastectomy Radiotherapy (PMRT)
- 31% pts undergoing mastectomy underwent post mastectomy radiotherapy (PMRT)
- Mx/ recon- 34% XRT, 66% no XRT
- Mx/ no recon- 20% XRT, 80% no XRT
| PMRT % of Mx |
Recon No XRT |
Recon XRT |
No Recon No XRT |
No Recon XRT |
|
| 2013 | 26 35 |
52 13 |
14 4 |
21 51 |
12 31 |
| 2014 | 24 34 |
64 12 |
12 4 |
24 52 |
12 30 |
| 2015 | 32 36 |
54 16 |
26 5 |
14 52 |
6 31 |
| 2016 | 24 35 |
67 15 |
18 5 |
9 48 |
6 30 |
| 2017 | 35 37 |
45 15 |
25 6 |
20 49 |
10 31 |
| 2018 | 31 | 52 | 27 | 17 | 4 |
Figures in red in table above are the corresponding Australasian figures from Breast SurgANZ Quality Audit.
The comparatively slightly lower overall rate of PMRT in my practice (31% in 2018) (compared to the national figures (37% in 2017) I think is likely to be a result of my pt demographics, with younger patients choosing mastectomy, often bilat, for preinvasive and low risk invasive disease, hence a lower proportion overall requiring PMRT.
The strikingly different percentages within the four categories in my practice c/w national averages is primarily related to a high rate of immediate recon in my practice (80%) compared with the Australasian average (21% in 2017) and the fact that I do not regard the need for PMRT as a reason to counsel patients against having an immed recon. 25% of my patients undergoing mx with recon underwent radiation compared to national average of only 6%.
| Chemotherapy % |
Radiotherapy % |
|
| All Mx | 52 | 31 |
| Mx with recon | 55 | 34 |
| Mx/no recon | 40 | 20 |
Summary:
- Stable, very high immediate reconstruction rate of 80% compared with the national average of approx. 20%
- Introduction of prepectoral implant- based reconstruction in 2018 (38% of all implant based reconstructions for cancer and 50% of all implant based reconstructions in association with risk-reduction mastectomy)
- Continued increase in the overall mastectomy rate (48% 2018, 40% 2016, 36% 2015)
- Continued Increase in bilateral mastectomy rate (45% of all Mx in 2018, 32% 2016, 28% 2015)
- Continued increase in the proportion of autologous reconstructions (82% of all immediate recons for malignancy, 33% of all immediate recons in association with risk-reducing mastectomy)
- Low mastectomy rate for involved margins (0%)
- Increasing use of neoadjuvant chemotherapy, with 300% increase over the last 5 years (14% in 2018 compared to 4% in 2013).
- Slight increase in % pts undergoing PMRT (31% in 2018 compared to 26% in 2013)
- No evidence to suggest that the need for chemotherapy OR radiotherapy is a deterrent to immediate breast reconstruction, and in fact the proportions of women undergoing chemotherapy and radiotherapy were higher in the setting of immediate reconstruction than without reconstruction.
In 2018 there was a 52% increase in the absolute number of reconstructive cases (excludes oncoplastic cases at time of breast conserving surgery).
This reflects several things,
- Increase in overall caseload, with more patients undergoing breast cancer or risk-reduction surgery than in any previous year.
- Increased mastectomy rate, and hence the absolute number of reconstructions (reconstruction rate has been fairly constant over last 3 years)
- Increase in the number of risk-reduction mastectomies
Discussion:
Unilateral/Bilateral Mastectomy Rates
The introduction of breast conservation as an alternative to mastectomy is attributed to clinical trials published in the 1980s. Multiple prospective randomized trials, now with long-term follow-up, have demonstrated that the survival rate after breast-conserving surgery (BCS) and whole-breast radiotherapy is equivalent to the survival rate after mastectomy.
In spite of this, a recent increase in rates of mastectomy, particularly in the United States, has been observed after years of steady decline. Studies have found a decline in breast conservation rates beginning in the early 2000s. Nationwide analyses of data demonstrated decreasing rates of mastectomy for early-stage breast cancer from the 1980s through the mid-2000s but subsequent increasing rates from 2005.
A retrospective cohort analysis using the ACS-NSQIP database from 2005 to 2016 reported a 49% mastectomy rate in 2016. (4)
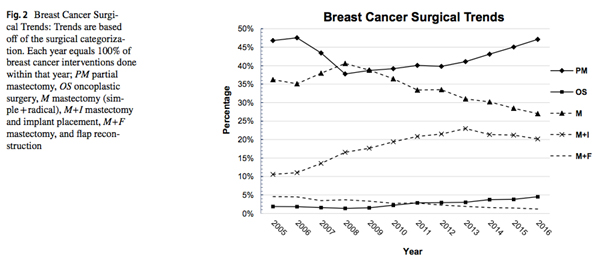
The observed increase in mastectomy rates is largely attributable to a rise in bilateral mastectomy for unilateral, early-stage disease. Studies point to physican recommendation, patient concern about recurrence, increased use of breast magnetic resonance imaging, and desire for symmetry as the primary reasons women undergo bilateral mastectomy. Patients without an identified high-risk genetic mutation have been found to overestimate their risk of contralateral breast cancer.
Increasing mastectomy rates in patients eligible for BCS have been associated with coincident increases in breast reconstruction and bilateral mastectomy. Women are increasingly opting for bilateral instead of unilateral mastectomies, even in the absence of a genetic predisposition or oncologic risk factor supporting the use of contralateral prophylactic mastectomy (CPM). In addition, rates of contralateral breast cancer have also decreased because of the widespread use of adjuvant systemic therapy for early-stage breast cancer, and there is no evidence that bilateral mastectomies with contralateral prophylactic mastectomy prolong survival for women with sporadic breast cancer.

The choice between BCS or unilateral mastectomy (UM) versus CPM is complex; studies have tried to explain the rationale and to elicit the drivers of the trend toward CPM. Treatment factors including magnetic resonance imaging at diagnosis, increase in the frequency of prior negative breast biopsies, and availability of immediate breast reconstruction (IBR) are associated with CPM. Younger age, White or non-Black ethnic origin, and private health insurance are also commonly cited.
There is no established “appropriate” mastectomy rate in early breast cancer, although the American National Accreditation Program for Breast Centres upholds as a criterion for centre accreditation that BCS be performed for at least 50% of patients with early-stage breast cancer
Furthermore, the steepest rises in mastectomy rates in the United States are seen in younger women with preinvasive disease, those with smaller tumours, and those with node-negative disease. This suggests an increasing influence of factors unrelated to disease burden or concern about attaining locoregional control in performance of mastectomy, particularly in younger women. Most important, younger age was associated with mastectomy and there was a disproportionate rise in bilateral mastectomies for unilateral, early-stage cancers.
Greater use of mastectomy, and particularly contralateral prophylactic mastectomy, have been associated with younger age at diagnosis, greater educational attainment and socioeconomic status, race, higher histologic grade, and in situ/preinvasive malignancy cancer, with an association between breast reconstruction and bilateral mastectomies with contralateral prophylactic mastectomy
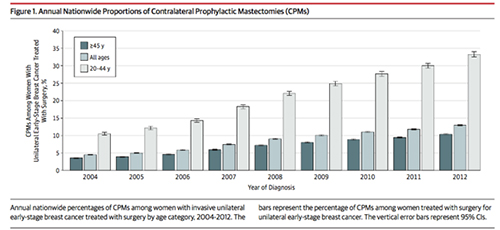
In an American cohort study of more than 1.2million women who received a diagnosis of invasive unilateral early-stage breast cancer treated with surgery, the proportion of contralateral prophylactic mastectomies varied substantially by state. The proportion among women 20 to 44 years of age during the period from 2010 to 2012 ranged from 15.7% in Hawaii to 42.8% to 48.5% in 5 contiguous Midwestern states. (1) JAMA Surgery 2017.
Surgical treatment for early-stage breast cancer is a “preference-sensitive” decision that should be made together by the patient and her breast surgeon considering individual clinical factors in conjunction with the patient’s values and preferences.
In breast cancer surgery, the quality of the decisions can be estimated by the extent to which patients are informed, involved in decision-making, and undergo treatments that reflect their values. Greater patient involvement has been associated with increased likelihood of mastectomy; The current patient-centred healthcare model has empowered patients to become active participants in their care decisions undergoing services based on individual needs/preferences.
Position statements as well as campaigns by the Society of Surgical Oncology and regulatory guidelines by American Society of Breast Surgeons have been created to address the increasing rate of CPM. There are however no established metrics for appropriate use of bilateral mastectomy.

In an effort to better understand why women increasingly choose CPM, health care providers are interested in better understanding its impact on health-related quality of life. The Mastectomy Reconstruction Outcomes Consortium carried out a multicenter prospective cohort study, which assessed patient-reported outcome along with the postoperative morbidity in women of 18 years and older with a diagnosis of unilateral in situ or invasive breast cancer. The results revealed that patients choosing CPM with bilateral implant-based reconstruction experienced significantly improved satisfaction with breasts as measured by the BREAST-Q along with reductions in anxiety and worry about future cancer episodes on the Generalized Anxiety Disorder 7 Scale and Patient-Reported Outcome Measurement Information System 29 anxiety inventories. Not surprisingly, CPM was associated with greater rates of complications whether a patient received prosthetic or autologous reconstruction. (2)
In a separate study (3) looking at the contribution of various factors, young age, and availability of IBR, explained the greatest variation in receipt of CPM. Other reasons invoked by patients who choose CPM pertain to psychological aspects of cancer such as fear of additional cancer episodes, peace of mind, and avoidance of future surveillance imaging.
The mastectomy rates rise after 2005 reflects a 14 percent annual increase in contralateral prophylactic mastectomies, as unilateral mastectomy rates did not change significantly. Each percentage point of increase in reconstruction rates was associated with a 7 percent increase in the probability of contralateral prophylactic mastectomies, with the greatest variation explained by young age (32 percent) and breast reconstruction (29 percent).
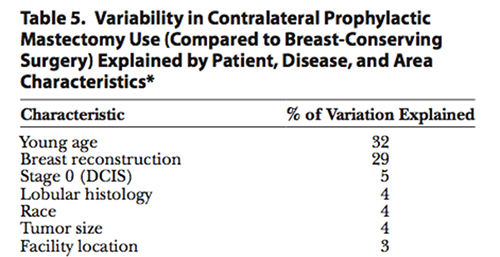
PRS 2015
The increased utilization of CPM raises ethical issue for physicians. In the current favoured patient- centred model oh healthcare, physicians are increasingly faced with the tension between honoring the patient’s autonomy to choose CPM and the goal to “ first, do no harm.”

Commentary:
- The mastectomy rate in Jane O’Brien’s breast surgical practice in 2018 (48%) is similar to the most recently reported rate in 2016 in the USA (49%) (4).
- 45% mastectomy patients underwent contralateral prophylactic mastectomy (CPM), which again is similar to the rate reported in 2012 in certain states of America (43-48%) (1)
There are several reasons a relatively high mastectomy/bilateral mastectomy rate in Jane O’Brien’s practice. The literature demonstrates that both young age and the availability of immediate breast reconstruction (IBR) are associated with an increased mastectomy rate, particularly bilateral mastectomy.
- 1. As Jane O’Brien has a special interest in the treatment of genetic breast cancer and breast cancer in younger women, she treats a disproportionate number of younger breast cancer patients.
Overall:
- 25 % breast cancers occur in women 50 and under (75% in women over the age of 50
- 11% breast cancers occur in women aged 45 and under
In 2018 in Jane O’Brien’s practice:
- 41% patients were aged 50 and under at the time of diagnosis
- 20% patients were aged 45 and under at the time of diagnosis ie almost double the expected %
- 2. Jane O’Brien has a special interest in immediate breast reconstruction (IBR), and a very high IBR rate (80%) compared to the national average (approximately 20%)
In 2018 in Jane O’Brien’s practice:
- 63% pts undergoing mastectomy with immediate reconstruction were aged 50yrs or under
- 35% were 45yrs or under
- 3. Referral patterns may also be significant. More than 30% patients who chose to have their breast cancer surgery performed by Jane O’Brien at St Vincent’s Private Hospital East Melbourne, are from outside Melbourne. She treats many “out of area” patients from regional Victoria, interstate and overseas and sees a lot of second opinions, many of whom specifically come to explore immediate reconstruction.
2018 Breast Cancer Patients (i.e. excluding risk-reduction surgery):
- 29% – Regional Victoria
- 3% – Interstate
- 2% – International
- 4. Studies have demonstrated greater use of mastectomy, and particularly contralateral prophylactic mastectomy, to be associated with younger age at diagnosis, greater educational attainment, socioeconomic status and private insurance. The sociodemographic features of Jane O’Brien’s patient population overlap with the factors known to be associated with higher rates of mastectomy/bilateral mastectomy and immediate breast reconstruction.
References:
1. Nash et al. State Variation in the Receipt of a Contralateral Prophylactic Mastectomy Among Women Who Received a Diagnosis
of Invasive Unilateral Early-Stage Breast Cancer
in the United States, 2004-2012. JAMA Surgery, 2017 ![]() Click here for more information
Click here for more information
2. Panchal et al. Current Trends in Postmastectomy Breast Reconstruction. Plastic and Reconstructive Surgery, 2017 ![]() Click here for more information
Click here for more information
3. Albornoz et al. Bilateral Mastectomy versus Breast-Conserving Surgery for Early-Stage Breast Cancer: The Role of Breast Reconstruction. Plastic and Reconstructive Surgery, 2015![]() Click here for more information
Click here for more information
4. Jonczyk et al. Surgical trends in breast cancer: a rise in novel operative treatment options over a 12 year analysis. Breast Cancer Research and Treatment, 2018 ![]() Click here for more information
Click here for more information
5. Read et al, Utility of neoadjuvant chemotherapy in the treatment of operable breast cancer. ANZ J Surg, 2015. ![]() Click here for more information
Click here for more information
6. Brittany L. Murphy and Judy C. Boughey, Changes in Use of Neoadjuvant Chemotherapy Over Time—Highest Rates of Use Now in Triple- Negative and HER2+ Disease, Ann Surg Oncol, 2018. ![]() Click here for more information
Click here for more information
You will need the Adobe Reader to view and print these documents.
![]()











